By David Hudnall, DMD
Any treatment has both pluses and minuses associated with it. Dental implants are no exception. When weighing their pros and cons, replacing missing teeth with implant-supported restorations generally offer many more advantages than disadvantages if utilized in conjunction with the proper clinical indications. That said, no treatment is perfect and it is possible for patients to suffer from a gum disease specifically associated with dental implants –– peri-implantitis.
What Is Peri-Implantitis?
Peri-implantitis is a destructive inflammatory disease process affecting the soft and hard tissues that surround previously osseointegrated dental implants. The condition is characterized by many of the same classic signs as periodontitis: soft tissue inflammation, bleeding with brushing or probing, purulence, and bone loss.
In the majority of cases, peri-implant mucositis occurs prior to peri-implantitis. This stage causes a localized inflammation at the junction of the implant with the soft tissue. Peri-implant mucositis can easily progress into peri-implantitis accompanied by recession and progressive alveolar bone loss. Left unchecked, peri-implantitis will eventually lead to implant mobility. Surgical entry into peri-implantitis sites often reveals a pattern of circumferential bone loss.
Symptoms of Peri-Implantitis
Clinical Signs
Because a clinical diagnosis of peri-implantitis involves inflammation of soft tissues and destruction of bone, there is usually evidence of bone loss observed on a routine radiograph and bleeding when the surrounding tissues are gently probed.
In the dental literature, there have also been reports of bone loss around an implant in the absence of any accompanying signs of soft tissue inflammation. Although, clinical evidence suggests that progressive bone loss around implants in the absence of clinical signs of soft tissue inflammation is a rare occurrence.
This disease phenomenon should not be confused with implants that fail to osseointegrate after placement. Peri-implantitis can occur at any time following dental implant integration. Clinicians should check the tissue surrounding implants for early signs of peri-implantitis by regularly monitoring changes in radiographic bone levels, probing depths, bleeding, swelling, suppuration, calculus buildup, and changes in tissue color.
Patient Symptoms
From the patient’s perspective, many patients don’t notice or ignore dental issues until they become glaringly obvious or cause pain. Just like with periodontitis (gum disease), patients who suffer from peri-implantitis are often unaware that an infection is present until it has progressed significantly.
Because the implant will still be fused to bone near the implant’s base even in the presence of coronal bone loss, it takes much more time for the patient to notice actual loosening or wobbling of the implant. By the time they observe this symptom, peri-implantitis has usually progressed to the point that implant failure is imminent.
The first thing a patient should be trained to look for is bleeding while cleaning around the implant. The patient may also become aware of puffy or swollen tissue surrounding the implant, bad breath, or a foul taste that they can’t seem to resolve. Early detection of peri-implantitis is critical. As soon as any of these symptoms are present, the patient should seek immediate treatment.
How To Prevent Peri-Implantitis
Strong evidence exists that there is an increased risk of developing peri-implantitis in patients who have a history of chronic periodontitis, poor plaque control skills, and no regular maintenance care after implant placement. Although data identifying smoking and diabetes as risk factors/indicators for peri-implantitis is somewhat inconclusive, there is no doubt that both have a compromising effect on the body’s ability to send agents involved in fighting harmful bacteria to areas of invasion via the circulatory and lymphatic systems.
Prevention is key. Patients and clinicians should be aware that once clinical signs of peri-implantitis develop and there is actual bone loss around an implant, the concept of the implant lasting for the length of the patient’s life goes out the window.
Long-term survival rates in clinical studies involving peri-implantitis patients receiving therapy are often discussed and measured in years, planning for alternative treatment when implant failure eventually occurs.
Steps To Prevent Peri-Implantitis:
- Maintain good oral hygiene at home
- Stop smoking
- Maintain control of diabetes and other chronic diseases
- Biannual professional implant cleaning and maintenance
These steps will help dentists to detect and prevent peri-implantitis while supporting the patient’s overall dental health. Of course, it can’t be stressed enough that many of these preventive steps are solely within the patient’s own control. The dentist can’t care about the patient’s best interest more than the patient does. The best thing a clinician can offer is to stress how daily maintenance and prevention are necessary in order to preserve the patient’s long-term investment of both time and money.
Peri-Implantitis Treatment
What should the dentist do when a patient presents with mucositis or bone loss around existing dental implants? What are the options for treatment? What types of treatment can be performed to eradicate the disease?
Non-Surgical Treatment
Peri-implant mucositis is treated with a thorough professional non-surgical cleaning followed by chlorhexidine mouth rinses and gels to decrease the bacterial count. It is also critical that the dentist or periodontist check for lingering deposits of crown and bridge cement beneath the gum tissue around the implant. The presence of dental cements is often a contributing factor in the development of peri-implantitis.
Re-evaluate the case after four to six weeks. If bleeding with tissue manipulation (brushing, gentle probing) has ceased and if the probing depths have also decreased, schedule the patient for recall appointments according to the professional’s assessment of the patient’s individual needs.
Following non-surgical treatment, antibiotics such as Metronidazole may be used to help alleviate lingering infection and improve tissue health. If mucositis is treated prior to bone loss, usually treatment will arrest the disease process before it has had the opportunity to progress into peri-implantitis.
Surgical Intervention
If the patient exhibits signs of bone loss with bleeding or pus that cannot be resolved with non-surgical therapy alone, surgical treatment should be employed. Depending on the amount of inflammation present, it may be prudent to repeat the non-surgical debridement one week prior to peri-implantitis treatment surgery in order to better control tissue bleeding and inflammation, making it easier to visualize the extent of destruction during surgery.
Options for Surgical Treatment.
The exact type of pre-implantitis treatment surgery will depend on the nature of the damage caused by peri-implantitis and will likely include a combination of surgical procedures to address the disease:
- Bone grafts to eliminate bony pockets and defects around the implant
- Resective surgery to remove bony ledges and flatten bone irregularities around the implant
- Implantoplasty to remove coronally-exposed threads on the implant itself, leaving a highly-polished implant surface
- Tissue grafts to increase the quantity of thick, non-mobile keratinized tissue around the implant
Many peri-implantitis cases are associated with a lack of an adequate quantity of soft tissue surrounding the implant. Thick, non-mobile keratinized tissue has been shown to decrease and actually prevent bone loss around implants. Soft tissue quantity can be improved with tissue grafts taken from the patient’s palate. Collagen-based grafts may also be used successfully as an alternative to reconstruct the soft tissues around implants.
Implant Removal
In cases involving severe bone loss, the implant should be removed entirely and bone grafted to fill in the void that remains to minimize further complications. The supplemental bone helps to boost the overall strength of the patient’s jaw and increase stability for potential implant replacement in the future. Again, antibiotics will aid in the healing process after treatment by eliminating harmful bacteria before it can spread to more remote areas of the bone.
The earlier that peri-implant mucositis and peri-implantitis are detected, the better the chances of successful treatment. But, better still is preventing the disease entirely through proper home hygiene and regular professional cleanings and maintenance of the teeth, implants, and gum tissues.
Restorations That Make Disease-Free Implants Look Great
For implant-retained restorations to be useful, they must be supported by stable implants that are free of disease. Stomadent Dental Laboratory offers many different restorative options to match your patient’s every treatment need, ranging from single crowns, to implant-supported dentures, to full-mouth bridgework.
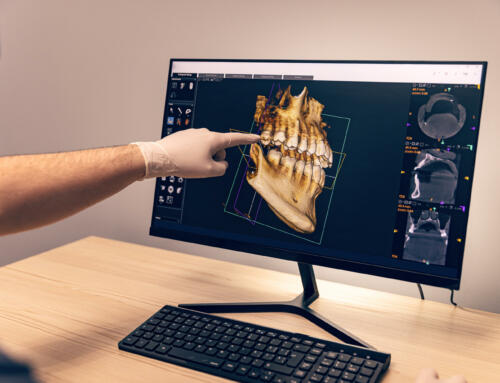
When it comes to CAD/CAM restorations with precise fit and impeccable beauty, trust Stomadent to deliver. To see the full line with pricing for implant-supported dental appliances, review Stomadent’s fee schedule.



![Hybrid Denture with Titanium Bar [Best Methods + Advantages]](https://stomadentlab.com/wp-content/uploads/2024/01/dental-prosthesis-on-dark-background-2023-11-27-05-06-28-utc-scaled-500x383.jpg)
![The Lucitone Denture Advantage [Best Practices + Advice]](https://stomadentlab.com/wp-content/uploads/2022/08/lucitone-promo-1-500x383.jpg)

![How to Remove Snap On Dentures [Expert Guidance]](https://stomadentlab.com/wp-content/uploads/2023/12/a-denture-in-a-glass-of-water-dental-prosthesis-c-2023-11-27-04-50-54-utc-scaled-500x383.jpg)